Educational Highlights

With the full commitment of our Sutter Health Family Medicine faculty and academic team, Residents will have the opportunity to provide patient-centered team-based care for all of Northern California's communities. Our exciting collaborations across departments, institutions, and participating teaching sites will provide innovative training that will prepare you for the future of family medicine.
Education and Community Involvement
Our residents are trained in all forms of contraception from LARCs (IUD, Nexplanon) to sterilization (vasectomy and postpartum tubal ligations). We have been the consult service at Sutter Medical Center Sacramento for Nexplanon implant placements for several years. We incorporate miscarriage management and abortion care into the continuity clinic medical home and have dedicated procedural clinics.
During residency, interested trainees can gain competency in medical and surgical TABs, miscarriage management, gynecological ultrasound, colposcopy and cervical biopsies, endometrial biopsies, IUD and Nexplanon insertions & removals, and LEEPs.
We offer a wide variety of educational experiences in obstetrical care thanks to our faculty expertise and strong support through our institution. Our goal is to provide residents with a positive OB experience and to graduate Family Medicine doctors who are competent and confident to take care of a broad array of OB patients. Our residents care for their own continuity patients in the clinic and deliver alongside our Family Medicine faculty as well as community OB/GYNs.
Residents who wish to continue performing OB deliveries after graduation can further enhance their experience through our Comprehensive OB track. This program offers opportunities to gain additional time on Labor and Delivery, where residents can work with high-risk OB patients and handle complex labor complications, including vacuum-assisted deliveries and more complicated vaginal lacerations. High-risk prenatal conditions include gestational diabetes, chronic hypertension, or patients seeking a trial of labor after a cesarean section. Residents participate in cesarean sections alongside our OB/GYN colleagues and several surgical FMOB faculty members.
After delivery, we continue to provide comprehensive care to both parent and baby. We promote postpartum contraception and family planning. We encourage breastfeeding among our new parents and are proud to say that both Sutter Medical Center Sacramento and Sutter Davis Hospital have been designated Baby Friendly Hospitals. Our residents can even do home visits for new parents with social challenges.
Best of all, we often become the doctors of the babies we deliver!

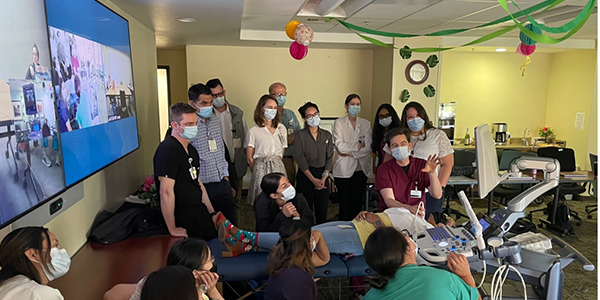
Point-of-care ultrasound can quickly answer a burning clinical question like is this baby breech, are there gallstones, is a DVT causing this leg swelling, and what is that lump under the skin? Our residents have access to multiple ultrasound devices including hand-held and cart-based machines both in the outpatient and inpatient settings. Sutter Health has an exclusive relationship with GE HealthCare for all ultrasound equipment, including a recent multiyear investment in AI technology. Our multiple VScan Air devices are especially helpful in facilitating workshops such as the workshop shown below where we reviewed shoulder & knee problems and injections.
Residents are trained in using ultrasound for not just prenatal purposes, but for IUD placement, abnormal vaginal bleeding, biliary disease, aortic aneurysm & vascular imaging, hydronephrosis, differentiation of cysts/masses/abscesses, chest diseases, FNAs, and for musculoskeletal imaging including joint aspiration/injection. We have regular workshops in didactics scanning each other and special workshops yearly with volunteer patients with significant findings. Bringing a handheld device on rounds is also a great way to appreciate POCUS findings on patients with significant pathologies.
We have an online POCUS training subscription for all residents and faculty accessible through the Global Ultrasound Institute (GUSI) .
Orthopedic Health
Sports Medicine provides advanced care not just for athletes, but for anyone who enjoys physical activity. It can help patients get back to the top of their game or simply back to the active life that they enjoy. Sports medicine primary care physicians help their patients improve performance, enhance overall health, prevent injury and maintain their physical activity throughout their lives.

At Sutter Health FMRP, we have multiple opportunities woven into our rotations to explore Sports Medicine and additional volunteer experiences as well. Notably, we have family physician Dr. Jeffrey Mann, board certified in Sports Medicine, who enjoys teaching musculoskeletal assessment, including POCUS evaluation, and management of MSK injuries and joint injections/aspirations. We also work with local teams (both collegiate and professional) in addition to organizations such as CIM (California International Marathon).
At the Sutter Health Family Medicine Residency Program, family physician Jeffrey Mann DO (Dr. Mann), board certified in Sports Medicine, enjoys teaching musculoskeletal assessment – including POCUS evaluation – and management of common and uncommon MSK injuries.
Goals of our Sports Medicine training include:
- Diagnosis and treatment of sports or activity-related injuries and illnesses.
- Use of manual techniques to prevent and treat musculoskeletal conditions common in athletes.
- Special knowledge of the principles of athletic conditioning.
- Focus on injury prevention and rehabilitation, including injuries common to specific sports.
- Nutritional guidance to build strength and endurance in support of athletic perform.

In addition to traditional allopathic medicine, our residency offers education in Osteopathic Manipulative Medicine. Both M.D. and D.O. residents will be educated on common musculoskeletal complaints, and how to use their hands to diagnose and help alleviate common conditions like back pain in pregnancy and tension headaches. Taught by a board-certified Neuromusculoskeletal Medicine physician Jeffrey Brodovsky, D.O., residents will gain valuable skills in manual medicine.

Furthermore, our program has Osteopathic Recognition. This allows M.D. and D.O. residents interested in osteopathic medicine the opportunity to take extra training throughout their 3 years to be eligible to sit for the osteopathic Family Medicine boards. These residents have their own osteopathic clinic, participate in osteopathic journal clubs, and receive additional preparation for osteopathic board certification.
Mental Health
We view Substance Use Disorder intervention as a core competency of any family physician. Our residency incorporates substance misuse (e.g. alcohol, tobacco, opiates, stimulants) in the longitudinal Human Behavior and Mental Health curriculum, as well as during the Psychiatry and Addiction Medicine rotations. During continuity clinic and inpatient rounds, residents gain experience in substance use disorder screening, intervention, and treatment – including Medication Assisted Treatment. We also have core faculty in the Motivational Interviewing (MI) Network of Trainers, who helps residents gain competency in this brief intervention.
Assisting patients with mental health issues, substance misuse, and behavior change are key elements in our Family Medicine clinics. To fully integrate the biopsychosocial model, our full-time behavioral scientist Dr. Sam Kettle regularly precepts with physician faculty during continuity clinic and inpatient rounds, and she is knowledgeable on vital community resources. This enables ongoing, real-time feedback about doctor-patient communication, contextual factors, psychosocial issues, and mental health disorders. We also have Behavioral Health Integration embedded in our continuity clinics with other mental health providers and navigators. Furthermore, residents can opt to use elective time for additional experiences in areas such as Addiction Medicine, Psychotherapy, Chronic Pain, Corrections Medicine, Lifestyle & Self-Management strategies, Spirituality in Medicine, and Well-being.
Other Education
Celebrating inclusion, belonging and encouraging all to be their most genuine selves is at the heart of our residency. We bring this philosophy with us when providing care to the transgender community — a traditionally marginalized patient population whose attempted suicide rates are close to 50%. Residents have the option to take a dedicated elective in gender-affirming care offered in our clinic in conjunction with the Gender Health Center, a local non-profit aimed at serving the transgender community. Through the elective, residents become proficient in hormone initiation and management, develop an understanding of ancillary community resources, and also learn how to navigate the often treacherous psychosocial waters that these patients must sail.
At its core, a family physician aims to relieve suffering. In June of 2016, California became the fifth state to legalize medical aid in dying. Through the End-of-Life Option Act, physicians are allowed to prescribe lethal medications to patients suffering at the end of their lives. Taught by faculty internationally-recognized for advocacy in this area, participating second and third year residents will have the opportunity to manage medical aid in dying in our clinic. Whether through in-office visits, telemedicine visits or home visits, residents help guide patients and their families through trying times and final hours with the utmost compassion and humanity.
We are proud of the communities we serve and the broad spectrum of care we can provide to our patients. As such, we are fortunate to have on staff Dr. Dineen Greer — an American Academy of HIV Medicine-certified HIV specialist. Through our HIV medicine elective, residents can become proficient in initiating and managing antiretrovirals, as well as managing complications from HIV/AIDS. Dedicated residents may be eligible to sit for their certification exams and become certified HIV specialists themselves.
Our program encourages residents to enhance appreciation and understanding of Integrative Medicine through mind, body, and spirit. Residents have the option to work with Sutter clinicians focusing in this approach (in both Sacramento and San Francisco), complete online courses, and/or attend a longitudinal or away elective such as the University of Arizona Integrative Medicine Rotation.
Practicing medicine is hard. Our program knows physicians are likely to develop many of their wellness patterns during residency just as they develop other behaviors that are part of medicine. These 3 years are the ideal time to facilitate development of well-being practices to have career-long impact. Therefore, we integrate wellness throughout the residency experience.
Residents enjoy having 2-week rotation blocks, jeopardy call, representation at faculty meetings – as well as easy parking and food at the physician lounge. We regularly offer support groups, Balint, cohort retreats, program retreat, wellness activities (such as yoga and narrative medicine), team building (e.g. volunteer at foodbank, float down the American River), and administrative support (e.g. ‘Friends with EPIC’/EHR, quality improvement of clinic operations). Our behavioral faculty are available at all times; as are senior residents, faculty advisors, and employee assistance program (EAP). There is also a Well-being elective to provide protected time for the resident to focus on creating a sustainable wellness plan for themselves and to model for patients .

Scholarly Activities and Research
We dedicate time and resources to promote research and scholarly activity among both resident and faculty physicians. During didactics, residents present journal club articles, as well as teaching a core Family Medicine topic. Sutter Medical Center Sacramento library personnel are available to assist with research and scholarly activities, as well as the staff at the Sutter Institute for Medical Research, and system-wide through Sutter Health’s GME Office of Academic Support. There is an annual Sutter Health-wide Research Symposium of posters and presentations to highlight research throughout the year from residents and faculty. Additional venues for submitting a poster presentation in which our residents have participated include the annual AAFP resident/student conference in Kansas City and the California Academy of Family Physicians’ annual Clinical Forum/Prism of Practice (POP ).
Specific didactics are provided each year to introduce these resources to our residents. In addition, residents may choose to participate in research studies and scholarly articles that residency faculty are undertaking.
Past projects include:
- Preconception CoIIN project – Investigate and innovate new approaches to pregnancy intention screening and follow up delivery in primary care setting
- The PATHFINDER study – A prospective study of 6,200 participants using the Grail multi-cancer blood test for screening and identification of multiple cancer types
- ROSES – A 3-year implementation study of ROSES, an evidence-based intervention to prevent postpartum depression in low-income women.
- Behavioral Health Integration (BHI) Project – Our Sacramento track received a large 2-year grant from DHCS to improve physical and behavioral health outcomes, care delivery efficiency, and patient experience by establishing fully integrated behavioral health care in continuity clinic (particularly for our patients with Medi-Cal). Faculty, residents & staff collaborate to establish this program and track. outcomes including healthcare access, population health metrics, patient improvement, and physician satisfaction.
- Medication Assisted Treatment (MAT) for SUD Project – Both our Sacramento & Davis tracks received 1-year grants from CAFP to improve integration of MAT in our continuity clinics. Our faculty, residents & staff work together to adjust clinic workflows to address substance use disorders in our patients, increase engagement, lower barriers to care, and improve patient outcomes.
- Interpersonal Violence Prevention (IPV) – Qualitative research exploring the impact of California’s physician IPV mandated reporting law.
Recent Publications by Faculty/Residents:
- Spielvogel R, Schewe S. Helping patients die: Implementation of a residency curriculum in medical aid in dying. Academic Medicine, 2024 Aug, 99(8): 863-867.
- Sullivan E, Stryker S, Blaszczak J, Spielvogel R, et al. Transgender care is Family Medicine: A call to action. Family Medicine, 2024 Apr; 56(4):229-233.
- Spielvogel R, Macmillan P. Current practices and future recommendations for graduate medical education in aid in dying. Journal of Aid in Dying Medicine, 2023 Dec; 1(1): 60-67.
- Spielvogel R, Stephens RB, Clark R, Guillen M, Hankins A, Parise C. Providing family planning counseling to women with chronic medical conditions in the acute care setting: A randomized feasibility trial. Contraception, 2023 Dec; 128:110133.
- Spielvogel, R. A hypervascular placental polyp after complete abortion: A case report. BMC Women’s Health, 2023 Oct; 23:534. https://doi.org/10.1186/s12905-023-02672-x
- Hitzeman N, Greer D, Carpio E. Office-Based Urinalysis: A Comprehensive Review. American Family Physician. 2022;106(1): 27-35.
Community Involvement
Community medicine is an inherent part of Family Medicine. Sacramento is one of the most diverse cities in the nation. As both a college town and agricultural hub, Davis also represents a wide range of cultures. Our continuity clinics and hospitals fully reflect the communities in which we practice. Our residents get robust experience working with patients of various languages, ethnicities, religions, sexual identities, socioeconomic statuses, gender identities, nationalities, indigenous heritages, and ages. In this way, community medicine is embedded within our continuity clinics. Our clinics are the foundational home of our training program. Residents spend an increasing amount of time within clinic during all three years, with direct observation, feedback, and guidance available at all times. All of our core physician faculty also have their own continuity clinic within the residency program clinics. This ensures a true primary care clinic experience for residents and mentorship by practicing physicians. Our primary care clinics are staffed with medical assistants, social workers, pharmacists, nurses, and health care coordinators to assure an integrated team approach.
In addition, we actively cultivate community partnerships as a residency and intentionally include resident training beyond our hospital and clinic walls. Some of our partners and collaborators are:
- Wellspace
- Communicare
- One Community Health
- Transitions
- Grant High School Sports Physicals
- Sacramento County Primary Health
- California Department of Corrections & Rehabilitation
- VA Northern California Health Care System
- La Familia
- Planned Parenthood
- Building Healthy Communities
- MACT Health Board
- Neighborhood Wellness
- Global Health: In past years residents & faculty have gone to Nicaragua, Tanzania, Ethiopia, India, Peru, and Thailand.
The Future Faces of Family Medicine project is a mentoring program set up by Sutter Health and UC Davis Family Medicine residents to inspire local high school students to become primary care physicians. The program has received statewide and nationwide attention.
Located in the capital of California, we have strategic proximity to our legislators, media hubs, and community initiatives. The voices of Family Medicine and our diverse patient population need to be heard more now than ever. Our faculty and residents are active in the community, and there are opportunities to get involved in local, state, and national efforts. Dr. Hitzeman is former editor and district board member at CAFP and encourages the entire FMRP community to participate in CAFP’s Annual Advocacy Day.

Dr. Spielvogel has been a champion of the End-of-Life Options Act (ELOA) since its enactment in 2016 and is a founding member of the ACAMAID (American Clinicians Academy on Medical Aid in Dying) national medical society. Dr. Spielvogel recently testified in the Scottish and UK Parliaments on End-of-Life and has been interviewed for a BBC documentary on the topic, set to air in 2025.
Drs. Brothers & Kettle work to ensure our Health Equity & Community Medicine curricula give a range of both high-level and hands-on experiences. Dr. Brothers has been Chair of Sutter Medical Group’s Inclusion and Belonging Taskforce. He has also worked with CMA to have our residents participate in their annual lobby day as well.

We are proud of our residents’ consistent engagement in community volunteering activities. Although residency is busy, we ensure there is spare time to volunteer at medical clinics for communities with limited access or limited resources, attend community meetings, and engage in meaningful activities as part of the larger community. We have regular protected afternoons for teambuilding activities, which often are chosen as group activities volunteering throughout local communities. We also partner with many community organizations to collaborate on improving the health of our neighborhoods and addressing social determinants of health on a more systemic level. Please see other sections and slideshows on our website for more information.
Unless we speak up in our community, our voices will not be heard, and the needs of our patients will not be met. Have you found your voice yet? Maybe we can help.
The Sacramento area is unique in that there are many Student-Run Clinics (SRCs) where local students and Family Medicine residents can volunteer. Traditionally, the Family Medicine residency programs in the area have been especially involved in the student-run clinics. As a resident, one finds that, after a short time, they can quickly pass on what they have learned to budding medical students. And the patients are so appreciative.
For more information on the local SRCs, please see theUC Davis School of Medicine.
To compare Sacramento’s abundance of SRCs with that of other cities around the country, please see the website for the Society of Student-Run Free Clinics.
Living in Sacramento
California's capital city is home to rural, suburban and urban neighborhoods, all with the mild climate California is famous for. Our dynamic downtown center is a hub for arts, music, theater, minor league sports and one of the largest urban recreational parks in the country.
Contact Us
Program Director
Ryan Spielvogel, M.D.
Program Administrator
Kenneth Enad
Sutter Health Family Medicine Residency Program
1201 Alhambra Blvd., Suite 340
Sacramento, CA 95816
916-731-7866
If you would like to correspond with our residents, please send your request to: sutterfmrp@sutterhealth.org
To reach the Alhambra Family Medicine Residency Clinic:
Patient Clinic Appointments: 916-451-4400
Clinic Fax: 916-731-7955




